- Visibility 171 Views
- Downloads 73 Downloads
- DOI 10.18231/j.ijcaap.2024.033
-
CrossMark
- Citation
Colonic drug delivery systems: Exploring the potential of biodegradable polymers for systemic effects
- Author Details:
-
Gangadi Jayapal Reddy *
-
Pavan Kumar Kokkula
-
M. Kannadasan
Introduction
Targeted drug delivery to the colon is highly desirable for treating various bowel diseases such as ulcerative colitis, Crohn’s disease, amebiasis, colonic cancer, and other colonic pathologies. It is also beneficial for the systemic delivery of protein and peptide drugs.[1], [2] A colon-specific drug delivery system (CDDS) must protect the drug during its journey to the colon, ensuring that release and absorption do not occur in the stomach or small intestine. The drug should only be released and absorbed once it reaches the colon.[3]
The colon is an ideal site for absorbing peptides and protein drugs for several reasons: it has fewer and less intense digestive enzymes, the proteolytic activity of the colon mucosa is much lower than in the small intestine, and the colon has a long residence time of up to five days, making it highly responsive to absorption enhancers.[4] This helps protect peptide drugs from hydrolysis and enzymatic degradation in the duodenum and jejunum, leading to greater systemic bioavailability.[5]
While the oral route is the most convenient and preferred for CDDS, other routes can also be used. Rectal administration offers a direct route to the colon but can be uncomfortable for patients and may not effectively target the proximal colon.[6] Intrarectal drug preparations, such as solutions, foams, and suppositories, are used for both systemic dosing and local treatment of the large intestine. The efficacy of these drugs depends on formulation factors, the extent of retrograde spreading, and retention time. Foams and suppositories are mainly retained in the rectum and sigmoid colon, while enema solutions have a greater spreading capacity.[7]
The colon’s high water absorption capacity and viscous contents can limit drug availability to the absorptive membrane. However, the colon’s diverse bacterial flora, with over 400 distinct species, can be leveraged for drug metabolism and targeted delivery of peptide-based macromolecules, such as insulin. These metabolic processes, including azoreduction and enzymatic cleavage, [8] can be applied to colon-targeted drug delivery, enhancing the effectiveness of treatments.
Factors to Consider in the Design of Colon-Specific Drug Delivery Systems Anatomy and Physiology of the Gastrointestinal Tract (GIT)
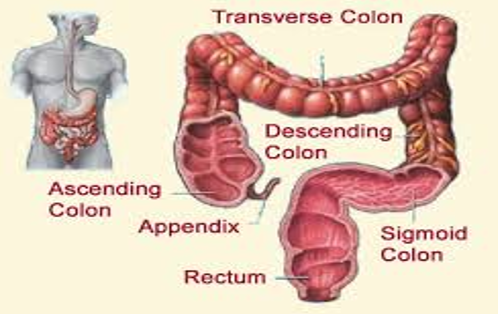
The gastrointestinal tract (GIT), also known as the alimentary canal, is a muscular digestive tube that winds through the body. It serves as a selective barrier between the external environment and systemic circulation. The GIT’s primary functions include digesting dietary food, absorbing nutrients, electrolytes, and fluids, and preventing the absorption of potentially harmful substances.[9]
The small intestine is the longest part of the GIT, where most enzymatic digestion and virtually all nutrient absorption occurs. The large intestine, the last major subdivision of the GIT, includes the cecum, colon, rectum, and anal canal. Understanding the anatomy and physiology of the GIT is crucial for designing effective colon-specific drug delivery systems.[10]
pH in the colon
|
Location |
pH |
|
Oral cavity |
6.2-7.4 |
|
Oesophagus |
5.0-6.0 |
|
Stomach |
Fasted condition: 1.5-2.0 Fed condition:3.0-5.0 |
|
Small intestine |
Right colon:6.4 Mild colon and left colon :6.0-7.6 |
Gastrointestinal transit
The gastric emptying of dosage forms is highly variable and primarily depends on whether the subject has eaten, as well as the properties of the dosage form, such as its size and density. The arrival of an oral dosage form at the colon is determined by the rate of gastric emptying and the transit time through the small intestine.[12]
|
Organ |
Transit time(h) |
|
Stomach |
<1(fasting) and, >2(fed) |
|
Small intestine |
3-4 |
|
Large intestine |
20-30 |
Colon bacteria
Nearly 400 distinct bacterial species have been identified throughout the gastrointestinal tract (GIT), with 20% to 30% belonging to the genus Bacteroides. The upper region of the GIT contains a relatively small number of bacteria, predominantly gram-positive facultative bacteria. The most significant anaerobic bacteria include Bacteroides, Bifidobacterium, Eubacterium, Peptococcus, Ruminococcus, Propionibacterium, and Clostridium.
The bacterial count (colony-forming units per milliliter, CFU/mL) in different regions of the GIT is as follows:
Stomach: 1 02-1 03 CFU/ml
Small intestine: 1 03-1 04 CFU/ml
Colon: 1 010-1 012 CFU/ml[13]
|
Target sites |
Disease conditions |
Drug and active agents |
|
Topical action |
Inflammatory Bowel Diseases, Irritable bowel disease and Crohn’s disease. |
Hydrocortisone, Budenoside, Prednisolone, Sulfaselazine, Olsalazine, |
|
Local action |
Chronic pancreatitis. Pancreatactomy and cystic fibrosis, Colorectal cancer |
|
|
Systemic action |
To prevent gastric irritation to prevent first pass metabolism of orally ingested drugs Oral delivery of peptides Oral delivery of vaccines |
Digestive enzyme supplements 5-Flourouracil. NSAIDS Steroids Insulin Typhoid |
Advantages of CDDS over Conventional Drug Delivery
Chronic colitis conditions, such as ulcerative colitis and Crohn’s disease, are typically treated with glucocorticoids and other anti-inflammatory agents. [13] However, administering glucocorticoids like dexamethasone and methylprednisolone orally or intravenously can lead to systemic side effects, including adenosuppression, immunosuppression, Cushingoid symptoms, and bone resorption. [12] Selective delivery of drugs to the colon can reduce the required dose and minimize these systemic side effects.[15]
Criteria for selection of drugs for CDDS
The best candidates for CDDS are drugs that show poor absorption from the stomach or intestine, including peptides. Drugs used to treat inflammatory bowel disease (IBD), ulcerative colitis, diarrhoea, and colon cancer are ideal for local colon delivery.[16] The criteria for selecting drugs for CDDS are summarized in [Table 4]. [17], [18], [19], [20]
Drug carrier selection for CDDS
The choice of drug carrier significantly influences the effectiveness of CDDS. The selection depends on the physicochemical nature of the drug and the disease being treated. Factors such as the chemical nature, stability, partition coefficient of the drug, and the type of absorption enhancer used are crucial in carrier selection. Additionally, the functional groups of the drug molecule play a role. For instance, aniline or nitro groups on a drug can be linked to another benzene group through an azo bond. Carriers containing additives like polymers, which may be used as matrices, hydrogels, or coating agents, can influence the release properties and efficacy of the drug delivery system. [16]
|
Criteria |
Pharmacological class |
Non-peptide drugs |
Peptide drugs |
|
Drugs used for local effects in colon against GIT diseases |
Anti-inflammatory drugs |
Oxyprenolo, Metoprolol, Nifedipine |
Amylin, Antisense oligonucleotide |
|
Drugs poorly absorbed from upper GIT |
Antihypertensive and antianginal drugs |
Ibuprofen, Isosorbide, Theophylline |
Cyclosporine, Desmopressin |
|
Drugs for colon cancer |
Antineoplastic drugs |
Pseudoephedrine |
Epoetin, Glucagon |
|
Drugs that degrade in stomach and small intestine |
Peptides and proteins |
Bromophenaramine, 5-Flourouraci, Doxorubicin |
Gonadoreline, Insulin, Interferons |
|
Drugs that undergo extensive first pass metabolism |
Nitroglycerin and corticosteroids |
Bleomycin, Nicotine |
Protirelin, sermorelin, Saloatonin |
|
Drugs for targeting |
Antiarthritic and antiasthamatic drugs |
Prednisolone, hydrocortisone, 5-Amino-salicylic acid |
Somatropin,Urotoilitin |
Primary Approaches for Colon-Specific Drug Delivery Systems (CDDS) pH-Sensitive Polymer Coated Drug Delivery to the Colon
In the stomach, the pH ranges between 1 and 2 during fasting but increases after eating.[21] The pH is about 6.5 in the proximal small intestine and about 7.5 in the distal small intestine.[22] From the ileum to the colon, the pH declines significantly, being around 6.4 in the cecum. However, pH values as low as 5.7 have been measured in the ascending colon in healthy volunteers. The pH in the transverse colon is 6.6 and 7.0 in the descending colon. [23] The use of pH-dependent polymers in colon-specific drug delivery is based on these pH differences. These polymers are insoluble at low pH levels but become increasingly soluble as the pH rises.[23] Although pH-dependent polymers can protect a formulation in the stomach and proximal small intestine, they may start to dissolve in the lower small intestine, leading to poor site-specificity.[24] Additionally, the decline in pH from the end of the small intestine to the colon can cause issues, such as lengthy lag times at the ileo-cecal junction or rapid transit through the ascending colon, resulting in poor site-specificity of enteric-coated single-unit formulations.[23]
Delayed (Time-Controlled Release System) Release Drug Delivery to the Colon
Time-controlled release systems (TCRS), such as sustained or delayed release dosage forms, are also promising for drug delivery. However, due to the potentially large variations in gastric emptying time of dosage forms in humans, the colon arrival time of these dosage forms cannot be accurately predicted, resulting in poor colonic availability.[25] These dosage forms may still be applicable as colon-targeting dosage forms by prolonging the lag time to about 5 to 6 hours.
Disadvantages of This System
Variable Gastric Emptying Time: Gastric emptying time can vary significantly between individuals and is influenced by the type and amount of food intake.
Gastrointestinal Movement: Gastrointestinal movements, especially peristalsis or stomach contractions, can alter the transit of the drug through the GIT.[26]
Accelerated Transit in Certain Conditions: Patients with inflammatory bowel disease (IBD), carcinoid syndrome, diarrhea, or ulcerative colitis may experience accelerated transit through different regions of the colon.[27], [28], [29]
Novel Colon Targeted Delivery System (CODESTM)
CODESTM is an innovative CDDS technology designed to overcome the limitations of pH or time-dependent systems. [30], [31] It combines pH-dependent and microbially triggered mechanisms. The system uses lactulose as a trigger for site-specific drug release in the colon. It consists of a traditional tablet core containing lactulose, coated with an acid-soluble material (Eudragit E), and then with an enteric material (Eudragit L). The enteric coating protects the tablet in the stomach and dissolves after gastric emptying. The acid-soluble coating then protects the preparation as it passes through the alkaline pH of the small intestine. Once in the colon, bacteria enzymatically degrade the lactulose into organic acids, lowering the pH around the system and dissolving the acid-soluble coating to release the drug. [32]
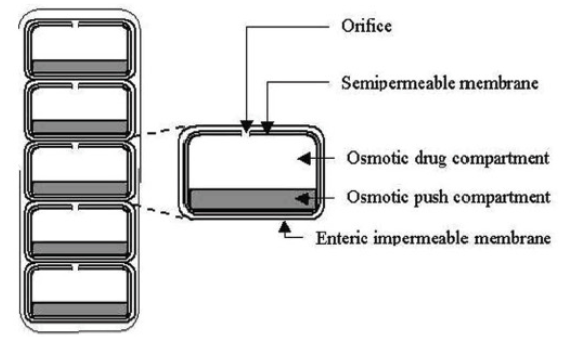
Osmotic Controlled Drug Delivery (ORDS-CT)
The OROS-CT system, developed by Alza Corporation, targets drugs locally to the colon for disease treatment or systemic absorption. [33] The system can be a single osmotic unit or include 5-6 push-pull units, each 4 mm in diameter, encapsulated within a hard gelatin capsule ([Figure 2]). [34] Each bilayer push-pull unit contains an osmotic push layer and a drug layer, both surrounded by a semipermeable membrane with an orifice next to the drug layer. After swallowing, the gelatin capsule dissolves, and the enteric coating prevents water absorption in the stomach. In the small intestine, the coating dissolves in the higher pH environment, allowing water to enter the unit, causing the osmotic push compartment to swell and create a flowable gel in the drug compartment. The swelling forces the drug gel out of the orifice at a controlled rate. For treating ulcerative colitis, each push-pull unit is designed with a 3-4-hour post-gastric delay to prevent drug delivery in the small intestine. Drug release begins in the colon, maintaining a constant release rate for up to 24 hours or delivering the drug over a shorter period.
Recent advancements in phase-transited systems show promise for targeting drugs to the colon.[35], [36], [37], [38] Various in vitro and in vivo evaluation techniques have been developed to test the performance and stability of CDDS.
In Vitro Models Used for CDDS
In Vitro dissolution test
The dissolution of controlled-release formulations for colon-specific drug delivery is complex, and the methods described in the USP cannot fully replicate in vivo conditions, such as pH, bacterial environment, and mixing forces.[32] Dissolution tests for CDDS can be conducted using the conventional basket method. Parallel dissolution studies in different buffers can characterize the behavior of formulations at various pH levels. For example, dissolution tests of colon-specific formulations in media simulating the pH conditions and times likely encountered in the gastrointestinal tract have been studied.[39] The chosen media include pH 1.2 to simulate gastric fluid, pH 6.8 for the jejunal region of the small intestine, and pH 7.2 for the ileum segment. Enteric-coated capsules for CDDS have been investigated in gradient dissolution studies in three buffers, tested for two hours at pH 1.2, one hour at pH 6.8, and finally at pH 7.4,[40]
In vitro enzymatic tests
Carrier drug systems are incubated in a fermenter containing a suitable medium for bacteria (e.g., Streptococcus faecium and Bacteroides ovatus). The amount of drug released at different time intervals is determined. Drug release studies are conducted in buffer media containing enzymes (e.g., pectinase, dextranase) or cecal contents from rats, guinea pigs, or rabbits. The amount of drug released over time is directly proportional to the rate of degradation of the polymer carrier.
In vivo evaluation
Various animals, such as dogs, guinea pigs, rats, and pigs, are used to evaluate drug delivery to the colon because their anatomical and physiological conditions, as well as their microflora, resemble those of the human GIT. When choosing a model for testing CDDS, it is important to consider models relevant to colonic diseases. Guinea pigs are commonly used for experimental IBD models. The distribution of azoreductase and glucuronidase activity in the GIT of rats and rabbits is comparable to that in humans. [41], [42], [43] For rapid evaluation of CDDS, a novel model has been proposed where the human fetal bowel is transplanted into a subcutaneous tunnel on the back of thymic nude mice. This bowel vascularizes within four weeks, matures, and develops a mucosal immune system from the host.
Conclusion
The colonic region of the GIT has become an increasingly important site for drug delivery and absorption. CDDS offers significant therapeutic benefits for both local and systemic treatments. Colon specificity is more likely to be achieved with systems that utilize natural materials degraded by colonic bacterial enzymes. Given the sophistication of colon-specific drug delivery systems and the challenges in establishing possible in vitro/in vivo correlations with current dissolution methods, pharmaceutical scientists face the task of developing and validating a dissolution method that incorporates the physiological features of the colon and can be routinely used in an industrial setting for evaluating CDDS.
Source of Funding
None.
Conflict of Interest
None.
References
- A K Philip, S Dabas, K Pathak. Optimized prodrug approach: A means for achieving enhanced anti-inflammatory potential in experimentally induced colitis. J Drug Target 2009. [Google Scholar]
- A O Oluwatoyin, T F John. In vitro evaluation of khaya and albizia gums as compression coating for drug targeting to the colon. J Pharm Pharmacol 2005. [Google Scholar]
- E O Akala, O Elekwachi, V Chase, H Johnson, Marjorie L Scott, K. Organic redox initiated polymerization process for the fabrication of hydrogel for colon specific drug delivery. Drug Dev Ind Pharm 2003. [Google Scholar]
- A Basit, J Bloor. Perspectives on colonic drug delivery. Business briefing. Pharmtech 2003. [Google Scholar]
- MK Chourasia, SK Jain. Pharmaceutical approaches to colon targeted drug delivery systems. J Pharm Sci 2003. [Google Scholar]
- P Watts, L Illum. Colonic drug delivery. Drug Dev Ind Pharm 1997. [Google Scholar]
- E Wood, CG Wilson, JG Hardy. The spreading of foam and solution enemas. Int J Pharm 1985. [Google Scholar]
- YW Chien. . Oral drug delivery and delivery systems 1992. [Google Scholar]
- L Liu, M Fishman, J Kost, KB Hicks. Pectin based systems for colon specific drug delivery via oral route. Biomaterials 2003. [Google Scholar]
- S K Vemula, P Reddy. Different approaches to design and evaluation of colon specific drug delivery system. Int J Pharm Technol 2001. [Google Scholar]
- Ysr Krishnaiah, Satyanarayana, Jain NK. . Advances in controlled and novel drug delivery 2001. [Google Scholar]
- AK Philip, RK Dubey, K Pathak. Optimizing delivery of flurbiprofen to the colon using a targeted prodrug approach. J Pharm Pharma 2008. [Google Scholar]
- AS Bansode, AB Athare, VS Kasture, PN Kendre. Colon targeted drug delivery system: An overview. Int J Pharm 2012. [Google Scholar]
- V R Sinha, R Kumar. Microbially triggered drug delivery to the colon. Eur J Pharm Sci 2003. [Google Scholar]
- SK Kulkarni, SK Kulkarni. . Handbook of experimental pharmacology. 1999. [Google Scholar]
- AD Mcleod, DR Friend, NT Thoma. Glucocorticoid-dextran conjugates as potential prodrugs for colon specific delivery: hydrolysis in rat gastrointestinal tract contents. J Pharm Sci 1994. [Google Scholar]
- SP Vyas, RK Khar. Gastroretentive systems. Controlled drug delivery: concepts and advances. 2005. [Google Scholar]
- K H Antonin, R Rak, P R Bieck, R Preiss, U Schenker, J Hastewell. The absorption of human calcitonin from the transverse colon of man. Int J Pharm 1996. [Google Scholar]
- J W Fara, Presscot LF, Nimmo WS. Novel drug delivery and its therapeutic application. Colonic drug absorption and metabolism 1989. [Google Scholar]
- M Mackay, E Tomlinson, Biek PR. . Colonic delivery of therapeutic peptides and proteins 1993. [Google Scholar]
- G V Mooter, C Samyn, R Kinget. . In vitro evaluation of a colon specific drug delivery system . [Google Scholar]
- A Rubinstein. Approaches and opportunities in colon-specific drug delivery. Crit RevTherap Drug Carrier Sys 1995. [Google Scholar]
- DF Evans, G Pye, R Bramley, AG Clark, TJ Dyson, JD Hardcastle. Measurement of gastrointestinal pH profiles in normal ambulant human subjects. Gut 1988. [Google Scholar]
- T Bussemer, I Otto, R Bodmeier. Pulsatile drug-delivery systems. Crit Rev Ther Drug Carr Sys 2001. [Google Scholar]
- M Ashord, JT Fell, D Attwood, H Sharma, P Woodhead. An evaluation of pectin as a carrier for drug targeting to the colon. J Control Rel 1993. [Google Scholar]
- A Gazzaniga, P Iamartino, G Maffino, ME Sangalli. Oral delayed-release system for colonic specific delivery. Int J Pharm 1994. [Google Scholar]
- E Fukui, N Miyamura, M Kobayashi. An in vitro investigation of the suitability of press-coated tablets with hydroxypropyl methylcellulose acetate succinate (HPMCAS) and hydrophobic additives in the outer shell for colon targeting. J Control Rel 2000. [Google Scholar]
- MS Reddy, RV Sinha, DS Reddy. Colon targeted systems. Drugs Today 1999. [Google Scholar]
- E Fukui, N Miyamura, K Verma, M Kobayashi. Preparation of enteric coated time released press coated tablets and evaluation of their function by in vitro and in vivo tests for colon targeting. Int J Pharm 2000. [Google Scholar]
- M Vassallo, M Camilleri, SF Phillip, ML Brow, NJ Chapman, GM Thomforde. Transit through the proximal colon influences stool weight in the irritable bowel syndrome. Gastroenterology 1992. [Google Scholar]
- MR Vonderohe, M Camolleri, LK Kvols, GM Thomforde. Motor dysfunction of the small bowel and colon in patients with the carcinoid syndrome and diarrhea. New Eng J Med 1993. [Google Scholar]
- S Takemura, S Watanabe, M Katsuma, M Fukui. Human gastrointestinal treatment study of a novel colon delivery system (CODES) using scintigraphy. Pro Int Sym Control Rel Bioact Mat 2000. [Google Scholar]
- K Masataka, S Watanabe, S Takemura, K Sako, T Sawada, Y Masuda. Scintigraphy evaluation of a novel colon-targeted delivery system (CODES) in healthy volunteers. J Pharm Sci 2004. [Google Scholar]
- L Yang, S James, A Joseph. Colon specific drug delivery: new approaches and in vitro/in vivo evaluation. Int J Pharm 2002. [Google Scholar]
- F Theeuwes, G Guittared, P Wong. . Delivery of drugs to colon by oral dosage forms . [Google Scholar]
- D Swanson, B Barclay, P Wong, F Theeuwes. Nifedipine gastrointestinal therapeutics system. Am J Med 1987. [Google Scholar]
- AK Philip, K Pathak. Osmotic flow through asymmetric membrane: A means for controlled delivery of drugs with varying solubility. AAPS Pharm SciTech 2006. [Google Scholar]
- AK Philip, K Pathak. In situ-formed asymmetric membrane capsule for osmotic release of poorly water-soluble drug. PDA J Pharm Sci Tech 2007. [Google Scholar]
- AK Philip, K Pathak, P Shakya. Asymmetric membrane in membrane capsules: A means for achieving delayed and osmotic flow of cefadroxil. Eur J Pharm Biopharm 2008. [Google Scholar]
- AK Philip, K Pathak. Wet process induced phase transited drug delivery system: A means for achieving osmotic, controlled, and level A IVIVC for poorly water-soluble drug. Drug Dev Ind Pharm 2008. [Google Scholar]
- IS Ahmed. Effect of simulated gastrointestinal condition on drug release from pectin/ethyl cellulose as film coating for drug delivery to the colon. Drug Dev Ind Pharm 2005. [Google Scholar]
- ET Cole, RA Scott, AL Connor, IR Wilding, HU Petereit, C Schminke. Enteric coated HPMC capsules designed to achieve intestinal targeting. Int J Pharm 2002. [Google Scholar]
- VG Mooter, R Kinget. Oral colon-specific drug delivery: A review. Drug Delivery 1995. [Google Scholar]
- Introduction
- Factors to Consider in the Design of Colon-Specific Drug Delivery Systems Anatomy and Physiology of the Gastrointestinal Tract (GIT)
- Advantages of CDDS over Conventional Drug Delivery
- Primary Approaches for Colon-Specific Drug Delivery Systems (CDDS) pH-Sensitive Polymer Coated Drug Delivery to the Colon
- Delayed (Time-Controlled Release System) Release Drug Delivery to the Colon
- Disadvantages of This System
- Novel Colon Targeted Delivery System (CODESTM)
- Osmotic Controlled Drug Delivery (ORDS-CT)
- In Vitro Models Used for CDDS
- Conclusion
- Source of Funding
- Conflict of Interest
How to Cite This Article
Vancouver
Reddy GJ, Kokkula PK, Kannadasan M. Colonic drug delivery systems: Exploring the potential of biodegradable polymers for systemic effects [Internet]. IP Int J Compr Adv Pharmacol. 2024 [cited 2025 Sep 12];9(4):221-226. Available from: https://doi.org/10.18231/j.ijcaap.2024.033
APA
Reddy, G. J., Kokkula, P. K., Kannadasan, M. (2024). Colonic drug delivery systems: Exploring the potential of biodegradable polymers for systemic effects. IP Int J Compr Adv Pharmacol, 9(4), 221-226. https://doi.org/10.18231/j.ijcaap.2024.033
MLA
Reddy, Gangadi Jayapal, Kokkula, Pavan Kumar, Kannadasan, M.. "Colonic drug delivery systems: Exploring the potential of biodegradable polymers for systemic effects." IP Int J Compr Adv Pharmacol, vol. 9, no. 4, 2024, pp. 221-226. https://doi.org/10.18231/j.ijcaap.2024.033
Chicago
Reddy, G. J., Kokkula, P. K., Kannadasan, M.. "Colonic drug delivery systems: Exploring the potential of biodegradable polymers for systemic effects." IP Int J Compr Adv Pharmacol 9, no. 4 (2024): 221-226. https://doi.org/10.18231/j.ijcaap.2024.033
